In a paper published online in the Proceedings of the National Academy of Sciences on November 23, 2020, Jun Yao of Tsinghua University and coauthors in China and the United States reported their findings in the mechanism underlying the induction of mania in bipolar disorder (BD), which is a neuropsychiatric disorder characterized by intermittent episodes of mania and depression.
The authors first analyzed the clinical pharmacological research in the past decades. 5-HT reuptake inhibitors (SSRIs) and NMDAR antagonists (e.g. ketamine) are two types of antidepressants that have distinct clinical performances. SSRIs cannot promote the mood of normal healthy people but it can treat major depression; however, in the treatment of bipolar depression, SSRIs often lead to mood overcorrection, which means the mood of the patients is switched from depression directly into mania or hypomania. The authors proposed that the mania and depression of BD might be the outcome of conflict between at least two systems that control mania/depression separately, rather than the regulation of one single pathway, and that is why SSRIs fail to brake. Furthermore, while ketamine can often induce manic or psychotic symptoms in individuals without mental illness, it has promising effects on bipolar depression patients without causing mood overcorrection. Not only ketamine but also other drugs targeting the glutamatergic system, such as lamotrigine and riluzole, do not have mood overcorrection effects either. Thus, the authors hypothesized that the target of ketamine, GluN2B-NMDARs, could be defective or inactive in BD patients, directly inducing antidepressant consequences; as a result, ketamine can only block the residual GluN2B activity in the patients to generate a moderate antidepressant effect, thus avoiding intense overcorrection responses. Based on this hypothesis, the authors investigated the mechanism of mania using Syt7 KO mice and BD patient iPSC-derived neurons.
Previously, Yao and Gage et al. have reported that Syt7 is key for the bipolar-like behavioral abnormalities in mice. In the present study, the authors first performed sequencing analysis in >1400 BD patients and >1200 healthy control subjects, and found several Syt7 SNPs in the patients but no Syt7 mutation was found in any healthy control subject, thus confirming the association of Syt7 with the susceptibility to BD in humans. Then, the authors treated Syt7 KO mice with Ro25-6981, a GluN2B-NMDAR antagonist similar to ketamine, and found that Ro25-6981 had robust effects on the wild-type mice but only showed moderate effects on the Syt7 KO mice. This result indicated that the authors’ hypothesis is probably correct. Then, the authors combined super-resolution STORM and SIM imaging techniques and the electrophysiological approach, and found that Syt7 and GluN2B-NMDARs were localized to the peripheral synaptic region, and Syt7 triggered glutamate release to efficiently activate the juxtaposed GluN2B-NMDARs. Thus, Syt7 deficiency and SNPs induced GluN2B-NMDAR dysfunctions in mice, and patient iPSC-derived neurons showed Syt7 deficit-induced GluN2B-NMDAR hypoactivity. The authors therefore concluded that Syt7 defects induced mania through attenuating GluN2B-NMDAR activity, which enabled the NMDAR antagonists to avoid mood overcorrection.
Dr. Jun Yao, from the State Key Laboratory of Membrane Biology, School of Life Sciences; Tsinghua-Peking Joint Center for Life Sciences, McGovern Institute for Brain Research, Tsinghua University; Dr. Qi Xu, from the Chinese Academy of Medical Sciences and Peking Union Medical College; and Dr. Fred Gage, from the Salk Institute for Biological Studies of U.S.A., are co-corresponding authors of the paper. Dr. Qiu-Wen Wang, Si-Yao Lu and Yao-Nan Liu, are co-first authors. All other co-authors made significant contributions to the paper.
Link to the paper: https://doi.org/10.1073/pnas.2016416117
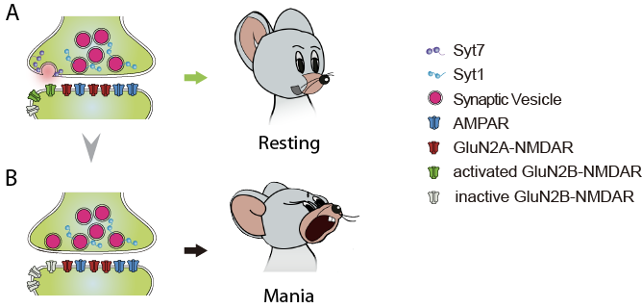
Figure 1. Syt7 deficits induce mania-like behaviors through GluN2B hypoactivity
